Does Top Dollar Equal Top Quality in VT Healthcare?
VHC911- Stat v.16
Recent Developments
VHC911 leaders Lisa Ventriss and Dr. Craig Jones joined Mark Johnson on WCAX's 802 News podcast for an in-depth conversation. They called for a leadership culture shift at the University of Vermont Health Network and discussed Vermont’s extraordinarily high healthcare costs and the dilemmas they pose for affordability and solvency. It’s a great, informative listen!
Last week, Vermont Public’s midday program, Vermont Edition hosted Dr. Sunil Eappen (UVM Health Network CEO), who stated that he “appreciates VHC911” and that “we are aligned on the overall goals of quality and affordability,” but we “differ on the data and sources of data” that VHC911 uses.
VHC911 will be able to say categorically that it is aligned with UVMHN on the matter of affordability and quality when we see real progress in both areas. With respect to data, coalition members and readers know VHC911 only uses credible, national data sources and audited financial statements. We will uncover and share more on any data “disagreements” in the months ahead.
The Green Mountain Care Board will approve hospital budgets and insurance premium rates by the end of September and we ask you to sign our petition against another double-digit rate increase for healthcare premiums.
High Prices, Average Quality
Of late, we’ve been digging into understanding how Vermont’s hospitals rank on quality compared to their peers. What we are finding is disappointing. Let’s start by reiterating what our research has revealed about prices overall: Vermonters pay among the most expensive health care prices in the nation.
Our families, in fact, spend more of their monthly household income on health insurance than any other state (Figure 1). Health insurance costs are nearly 20% of the median monthly household income in Vermont, while only 4% in New Hampshire. Considering that Vermont and New Hampshire patients share a border (and the Dartmouth Hitchcock Medical Center), these results are hard to justify.
Figure 1. Cost of Insurance as a Percentage of Median Monthly Household Income
Mediocre Quality Outcomes at VT’s Six Largest Hospitals
High insurance costs are record-setting in Vermont. But could that be because we are getting better quality for our premium dollar than our counterparts in New Hampshire and other states? In other words, do high prices correlate with improved quality across the board? Sadly, no.
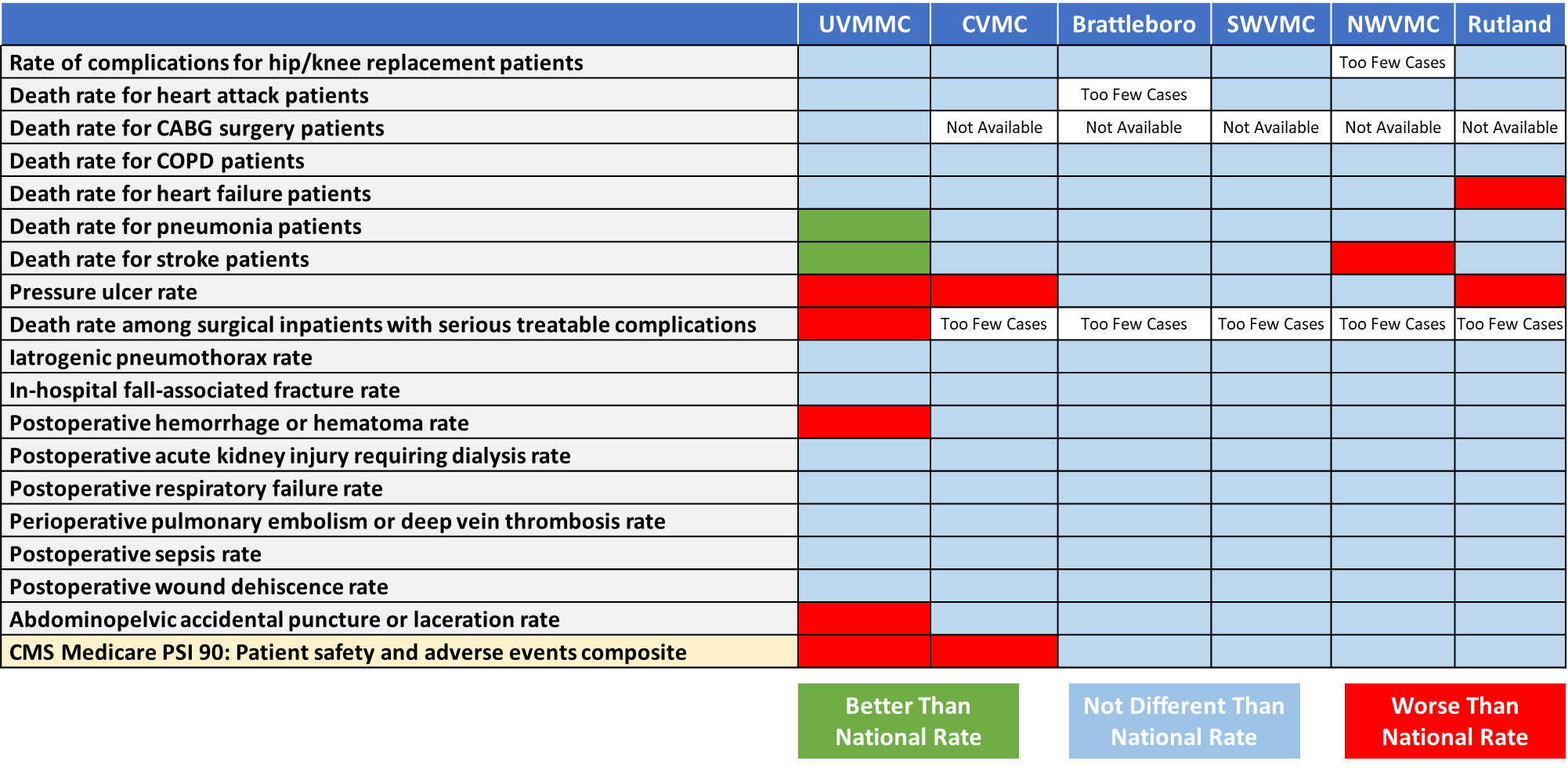
To understand why, we studied national quality assessments provided by The Centers for Medicare & Medicaid Services (CMS) that reflect their most recent reporting period ending 6/30/2023. CMS evaluates hospital quality each year and the results are made available publicly to support transparency and the public’s ability to choose healthcare providers (Hospital Quality Initiative Public Reporting | CMS).
Safety and mortality measures for Vermont’s largest six hospitals are shown in Table 1 below. Examples include “complications from hip and knee replacements,” “death rates for heart failure patients,” and “bone fractures for in-hospital falls.” Also included is the CMS Patient Safety and Adverse Events Composite (CMS PSI 90), which condenses a subset of indicators to summarize patient safety, monitor performance over time, and support comparative reporting and quality improvement at the hospital level (CMS Patient Safety Indicators PSI 90 Fact Sheet). CMS’s rankings are standardized to allow for a fair comparison nationally, and are presented by color:
Better Than the National Rate
Not Different Than the National Rate
Worse Than the National Rate
Quality Results at Vermont’s Six Largest Hospitals
Table 1 reveals that Vermont’s six largest hospitals are generally “average” with respect to 18 quality measures (“average” simply means they are in line with the national rate).
Importantly, UVMMC and CVMC, two of the three UVM Health Network hospitals in Vermont, have Patient Safety & Adverse Events Composite results (PSI 90) below the national rate. These are important measures (see Table 2) and include conditions like: bed sores (pressure ulcers), post-surgical infections and bleeding, organ failure, and surgical mistakes such as accidental punctures.
Healthcare workers often describe a challenge instituting practices to improve quality. This stems from multiple layers of management and an increasingly centralized decision-making structure meaning leadership is removed from the day-to-day operations at the hospitals. Effective, value-based models usually take the approach of empowering local teams to take ownership over improving outcomes on priority quality measures, and minimizing vertical management layers between local teams and organization leadership.
Table 1. Patient safety and mortality measure results for Vermont’s six largest hospitals.
While most of the quality measures are no different than the national rate, only Brattleboro and SWVMC in Bennington hit the national rate in every category. Each of the other four hospitals have safety and/or mortality rates that are worse than the national rate and, thus, should be a focus of quality improvement. Specifically, “death rates for heart failure” (Rutland), “death rates for stroke” (NWVMC), “pressure ulcers” (UVMMC, CVMC & Rutland), and “death rate among surgical inpatients with serious treatable complications” (UVMMC).
Of the six largest hospitals in Vermont, only UVMMC earned rankings above the national rate. At the same time, UVMMC also earned the most ratings in red (“worse than the national rate”).
Table 2. Indicators included in the PSI 90 composite (Patient Safety & Adverse Events).
Hospital-Acquired Infections
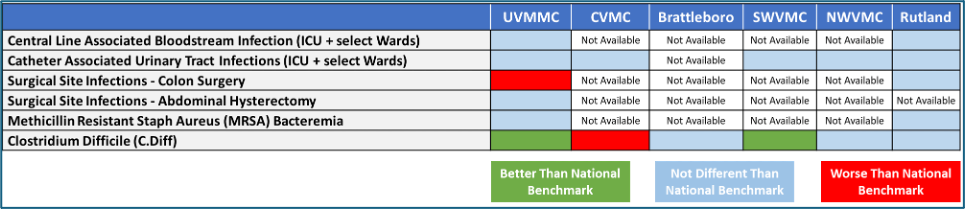
Results for hospital-associated infections as reported by CMS (Table 3) are somewhat difficult to assess because four (4) of our five (5) community hospitals are not reporting data. It’s tempting to think this is because of hospital size, but “Too Few Cases” is a reporting option. In fact, Rutland Regional Medical Center, our second largest hospital, reports on most of the CMS measures, indicating that reporting is feasible.
These results highlight that UVMMC and SWVMC are performing better than the national benchmark for bacterial infections of the colon spread from contaminated surfaces and objects (C Diff infections). It also shows opportunities for improvement with C. Diff infections at CVMC and a high rate of Surgical Site Infections following colon surgery at UVMMC.
Table 3. Hospital associated infection measure results for Vermont’s six largest hospitals.
Part of an overarching quality initiative in Vermont should be to understand why measure results are not reported when there may be an adequate number of cases. And we should promote better consistent reporting across hospitals.
In summary, most measures on safety, mortality, and infection for Vermont’s 6 largest hospitals are rated average. That might be more acceptable if our costs were also average. But, VHC911’s analysis do not indicate a high-value healthcare system. There is a clear imperative for hospital and health system leaders to develop strategies for improving quality. We can do better than average.
Vermont is heading into a consequential period with an intense focus on financial sustainability for the state’s small and mid-size hospitals. And a similarly intense focus on lowering the state’s high healthcare costs that are primarily driven by the UVM Health Network. In order to provide value to Vermonters, there needs to be a similarly intense focus on preserving and improving quality as hospitals reduce costs and transform their operations.
VHC911 is dedicated to helping Vermonters understand the need for hospitals to address both cost and quality, and to find opportunities for a purposeful shift to a value-based healthcare system in Vermont. This will require a change in the direction our hospitals have been trending in for several years, which have led to high costs, financial instability, and lower quality outcomes. There must be a fundamental change in medical and community priorities at several hospitals, including the UVM Health Network. Executive leaders and Boards of Directors must acknowledge the problems with cost, access, and quality and prioritize substantial changes in business operations and current cultures of leadership.