It's time to move past three tired excuses
VHC911 – Stat v.21
Long-Held Beliefs About Healthcare Costs Don’t Hold Up
As Stat readers know, Vermont has the highest commercial insurance rates in the nation. We can credit a prolonged period of poor oversight, lax accountability, price gouging, and asset hoarding by some hospitals for much of this crisis.
Adding to that, the state’s largest insurer, BCBSVT failed to negotiate aggressively with the UVMHN over prices. According to BCBS-VT, UVMHN had taken the position that if their rate demands were not met, they would stop seeing BCBSVT patients.
All in all, leaders and regulators failed to focus on costs and Vermonters are left paying the bill.
But new leaders are in place and opportunities are clear. Dr. Steve Leffler is the new CEO at UVMMC and the Network. Beth-Ann Roberts is the new CEO at Blue Cross VT. Both speak of a desire for affordability and sustainability, recognizing how out of balance our health system has become.
For future healthcare transformation work to be successful, and for healthcare to be far more affordable for all Vermonters, a new culture of price regulation, leadership engagement and accountability is essential.
Hospital Leaders Must Move Past Excuses that Justified the Current Crisis
For years we have heard that Vermont’s high healthcare costs are due to reasons we can’t control. Many argue that hospitals’ costs are high because Vermont has one of the oldest populations in the country.
Additionally, we hear, hospitals must charge high rates to commercial insurers because Medicare reimbursements to Vermont’s hospitals are some of the lowest in the country.
And, we hear Vermont seniors use a lot of healthcare.
Taken together, these create a trifecta of excuses: lots of seniors, low reimbursement from Medicare, and patients that use a lot of services. It’s no wonder healthcare is so expensive in Vermont.
Too bad the facts don’t support these assertions. They should be left in the past.
Take a look.
Vermont Medicare Patients Actually Have Low Per Capita Health Care Spending
We often hear healthcare leaders say Vermont seniors use a lot of healthcare.
A recent report by the Commonwealth Fund found that Medicare spending per beneficiary ranked Vermont 5th lowest of all the states. That makes claims of high utilization difficult to justify. The same report gave Vermont high rankings on performance indicators including avoidable unnecessary hospitalizations and the ability for Medicare patients to receive care when needed. The study ranked Vermont poorly (48th) when looking at “potentially avoidable emergency department visits” which obviously increase costs for our system. Still, on the whole, there is nothing here that suggests Vermont’s Medicare patients are high users of healthcare.
Vermont’s Population Age Distribution Does Not Explain Our High Costs
Vermont’s older population is a go-to excuse when hospitals explain the need for high charges to commercial insurance.
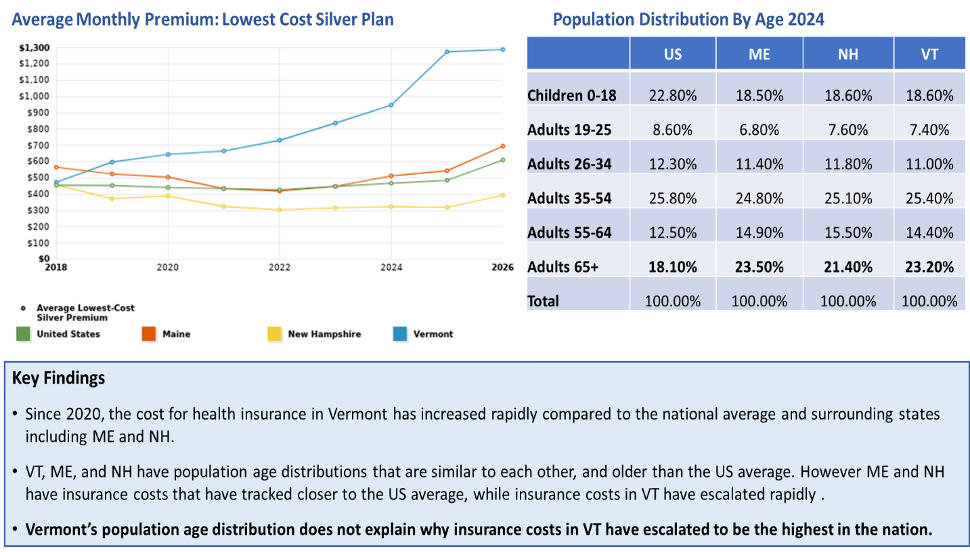
Vermont’s population is older than the US average. But Maine and New Hampshire are similarly older than average, with age distributions almost identical to VT. And all three northern New England states have similar proportion of our population aged 65+ years and covered by Medicare (Figure 1).
However, the growth of commercial insurance rates in ME and NH has remained similar to the US average while Vermont’s has escalated sharply since 2018.
In New Hampshire, commercial insurance costs are lower than the US national average and the state has the lowest proportion of monthly income that goes to pay for health insurance, while VT has the highest. Vermont is, on average, slightly older than New Hampshire but nothing that comes close to explaining these cost deviations.
Figure 1. Relationship between the cost of insurance and population age distribution
Medicare Inpatient Payments to Vermont Hospitals are Actually the 9th Highest in the Country
Vermont’s hospitals often say they receive some of the lowest Medicare reimbursement rates in the nation but we have not been able to find evidence to back up that claim.
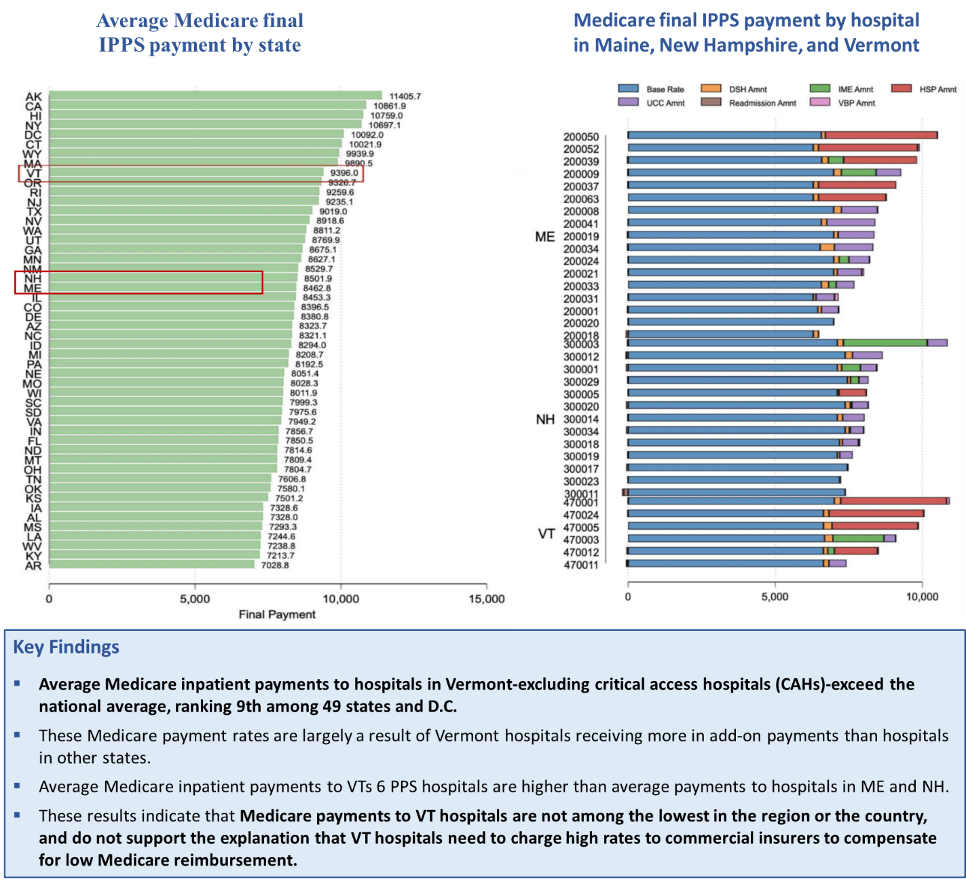
In November 2025, a team of economists at the Center for Advancing Health Policy through Research (CAHPR) at the Brown University School of Public Health produced an analysis of Medicare Final Payment Rates in Vermont for the Green Mountain Care Board (GMCB). The analysis showed that average Medicare inpatient payments to Vermont hospitals (excluding critical access hospitals) exceeds the national average and ranks 9th highest among 49 states and the District of Columbia (Maryland is excluded from the analysis due to operating under global budgets).
Medicare payments are comprised of a base rate plus add-on payments for factors such as the local wage index, the number of low-income patients, whether a hospital is a teaching hospital, adjustments for geography, use of a certified electronic health record, and incentive payments or penalties based on quality performance.
The high level of Medicare payment rates to Vermont’s 6 non-critical access hospitals were largely a result of Vermont hospitals receiving more in add-on payments than hospitals in other states (Figure 2). In contrast to the long-standing explanation offered by Vermont’s providers, these data findings are consistent with other national reports showing that VT does not receive low reimbursement from Medicare. Thus, this cannot explain why hospitals need to charge high rates to commercial insurers.
It is notable that this analysis also shows that ME and NH both receive lower Medicare payment rates than VT, yet they both have more affordable health insurance.
Figure 2. Medicare inpatient payments to hospitals in Vermont and across the nation
Vermont Has the Fourth Highest Per Capita Spending on Hospitals in the Nation
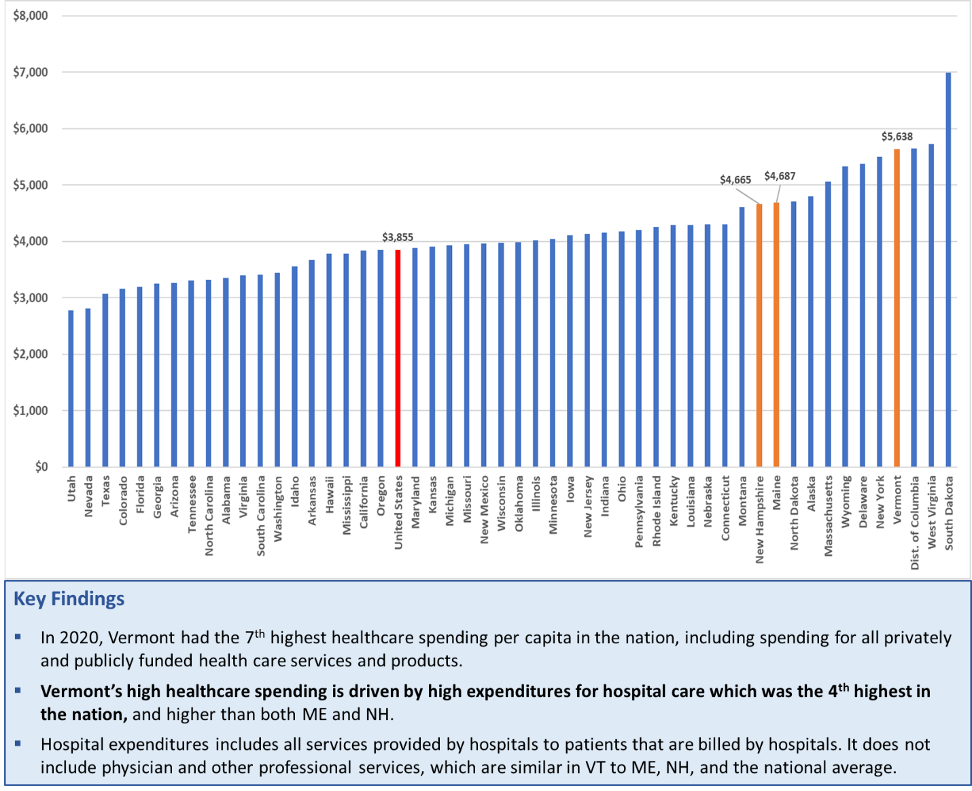
The underlying cause for high healthcare costs in VT is hospital spending – especially at our largest hospitals. This is reinforced by national data on healthcare expenditures per person across the country (Custom State Reports | KFF).
In 2020, Vermont had the 7th highest overall healthcare spending per person of any state in the country, with the 4th highest hospital spending per person of any state in the country (Figure 3). These findings include all public (Medicare and Medicaid) and private (commercial) healthcare spending for all services and products. The 2020 data is the most recent data available from the Kaiser Family Foundation (KFF), which is made available by CMS and updated every 5 years.
In other words, reducing health costs in Vermont will require greater efficiency from our hospitals and strategies that deliver care in appropriate settings outside hospitals.
Figure 3. Hospital Expenditures per Capita 2020
We Have the Means to Reduce Hospital Spending: Leadership, Statutory & Regulatory Framework, and One-Time Resources
The leadership teams at Vermont’s hospitals are deeply committed to serving their communities and providing Vermonters with the services they need. They have complex jobs leading institutions that are often the largest employer in their communities.
Just the same, it is important for these leaders to openly acknowledge the need for robust transformation and to work together in more cost-effective ways to deliver affordable care and to improve access, quality, and safety.
As we look to the future, we hope hospital leadership teams will reject tired excuses for our high costs that aren’t supported by data.
Several Reasons to Believe the Tide is Turning
The legislative reforms passed in 2025, combined with GMCB regulation and care transformation planning now being facilitated by the Agency of Human Services (AHS) will be supported in 2026 and beyond with substantial new funding from the Rural Health Transformation Program (more on this below). GMCB Chair Owen Foster did a good job explaining the opportunities last week on VT Public.
Act 68 of 2025 mandates that the Care Board implement reference-based pricing by fiscal year 2027, setting payments for hospital services pegged to Medicare rates (or other appropriate benchmarks). This is a critical first stage to establish hospital global budgets, also mandated by Act 68
Additionally, GMCB has an independent liaison team working directly with the UVM Health Network to lower costs and improve efficiencies. The liaison team has begun to report on progress, opportunities, and challenges as the UVM Health System reorganizes its operations under its new CEO, Dr. Stephen Leffler.
At the same time, AHS is working with all Vermont hospitals on care transformation plans, including strategies to institute cost savings by sharing and coordinating services on a regional basis. This transformation work will require hospitals to coordinate in new ways to reduce operating costs while improving quality and access. For example, hospitals can adopt shared administrative platforms, shared electronic health records, shared teams of clinical providers, expanded telehealth capabilities between larger and smaller hospitals, enhanced transfer and transportation capabilities, enhanced mobile health services, an expanded foundation of advanced primary care with integrated mental health and substance use services, and an expanded workforce.
In December 2025, Vermont was awarded about $195 million for 2026 to support these types of investments, with additional funding available for up to 5 years. This federal grant offers a unique opportunity to make critical investments in the transformation of our healthcare system.
The Green Mountain State is at an inflection point, and Vermonters should expect substantive and meaningful changes beginning in 2026 and continuing in subsequent years. It is essential that Vermonters stay informed and expect accountability and transparency from our state leadership and regulators.
VHC911 will continue to offer a forum to raise awareness and use data to support public understanding of how the state’s transformation work and reforms are progressing and their impact on ending the healthcare affordability crisis in our state.
Vermont Healthcare 911 (VHC911) is a broad coalition united to combat the high cost of healthcare in Vermont. The coalition is comprised of business owners, labor leaders, healthcare providers, civic and political leaders of all parties and represents over 200,000 Vermonters.